Stem cell therapies are advancing but will Australian patients be left behind?
Australia needs to develop new and better mechanisms to translate stem cell research into effective therapies, write Martin Pera, Megan Munsie and Richard P Harvey.
Australia needs to develop new and better mechanisms to translate stem cell research into effective therapies, write Martin Pera, Megan Munsie and Richard P Harvey.
OPINION: Discoveries in stem cell science over the past decade are finally starting to reach the clinic. Current clinical trials are evaluating stem cell therapies for conditions ranging from eye disease to AIDS.
These trials are going on in the United States, Europe, Canada, Japan and elsewhere. But Australia is lagging behind. While we remain fairly competitive in fundamental research, we are slow to translate our discoveries into new therapies.
This concern was expressed in the Australian Academy of Science report, released today, called The Stem Cell Revolution: Lessons and Imperatives for Australia. It contains a series of recommendations from young research leaders in the field on how Australian science policy can help fast-track stem cell research here.
Researchers are often asked by patients or their relatives when stem cell treatments will be available for certain medical conditions. Ten years ago, the answer would have been that there are no new treatments yet, but we are working to develop them. Today, we are forced to answer that clinical trials of cell therapies for particular conditions are going on, but not in Australia.
We have an obligation to ensure that Australian patients, their families, carers and physicians are not left behind in the stem cell revolution.
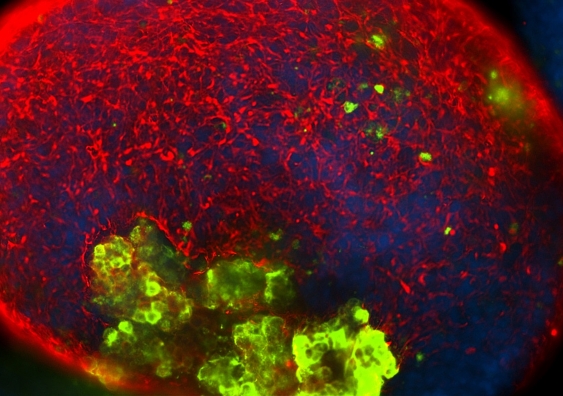
Human embryonic stem cells, which can become cells in any tissue of the body, were first discovered in 1998. Today, embryonic stem cell treatment trials are underway for macular degeneration (a common form of blindness), spinal cord injury, juvenile diabetes and heart failure.
Then there are the induced pluripotent stem (iPS) cells that Japanese scientist Shinya Yamanaka discovered, which won him the Nobel Prize in 2012. iPS cells are made from adult tissues and have many of the defining properties of embryonic stem cells. They can be made from skin or blood cells of any person.
After Yamanaka’s discovery, Japan’s cell therapy regulatory framework was modified to fast-track products from these new stem cells into the clinic. As a consequence, therapies using induced iPS cells, which enable close tissue matching of stem cell transplants to patients to prevent graft rejection, are now in clinical trials there, only ten years after their discovery.
More trials will begin very soon. For instance, years of research on midbrain dopaminergic neurons, the cells lost in Parkinson’s disease, has paved the way for upcoming trials of stem cells replacing these lost neurons.
There are also a large number of human trials in progress using mesenchymal stem cells, which are extracted from bone marrow, fat or other tissues. Capable of modulating the immune system and inflammatory response, these stem cells have the potential ability to treat arthritis, autoimmune disorders, graft versus host disease in bone marrow transplant patients, and a number of other conditions.
Neural stem cells derived from either foetal or adult brain tissue are also undergoing testing in humans, for rare inherited disorders of the brain or more common conditions including spinal cord injury.
It’s unlikely these early stage trials will produce cures for any of these conditions. Indeed they might pose as many questions as they answer. But it is essential and significant that these trials are moving forward, because the lessons we learn from them will guide us towards the design of the next generation of cellular therapeutics.
Today, genetic modification of stem cells with precision can provide cell therapies that can permanently correct serious genetic disorders.
For years, progress in gene therapy was almost totally blocked by safety concerns around the relatively crude technologies for introducing genetic alterations into patient cells. But technological advances have enabled precise correction of genetic defects within a cell. This avoids off-target modifications that can cause cancers and other serious toxicities.
New treatments using combined gene and cell therapy are undergoing trials now. The California Institute of Regenerative Medicine lists about ten new human studies, including in AIDS, blood diseases and cancer.
Then there is a third stream of stem cell research that, although perhaps less visible to the general public, has implications well beyond cell therapy.
This is the ability to derive pluripotent stem cells from patients with genetic predisposition to disease, or to introduce disease mutations into stem cells via gene editing. We can then use these disease-specific stem cell lines to generate the cell types affected in a particular disorder to study what goes wrong with them in the lab.
For instance, we can study how a gene that causes epilepsy affects the electrical properties of human nerve cells. Once we develop these cell culture models, we can use them to screen candidate drugs to correct the deficits in the affected cells.
This technology will enable us to reduce dependence on animal models, which don’t always replicate human diseases, and will reduce the risk of testing drugs on living human subjects.
These advances have the potential to speed the discovery of new medicines, to rapidly eliminate candidate drugs that might cause toxicity in the clinic, and to save millions from the costs of drug development.
To ensure Australian patients have timely access to new stem cell therapies for intractable diseases, we must maintain our excellence in fundamental stem cell research. But we also need to develop new and better mechanisms to support collaboration between academia, the private sector and philanthropists with the aim of translating discoveries into cures.
Martin Pera is Professor and Program Leader of Stem Cells Australia, University of Melbourne. Megan Munsie is Head of Education, Ethics, Law & Community Awareness Unit, Stem Cells Australia, University of Melbourne. Richard P Harvey is Professor, Victor Chang Cardiac Research Institute, UNSW.
This opinion piece was first published in The Conversation.