‘Animal Farm’ immunity receptors only work in a crowd, researchers find
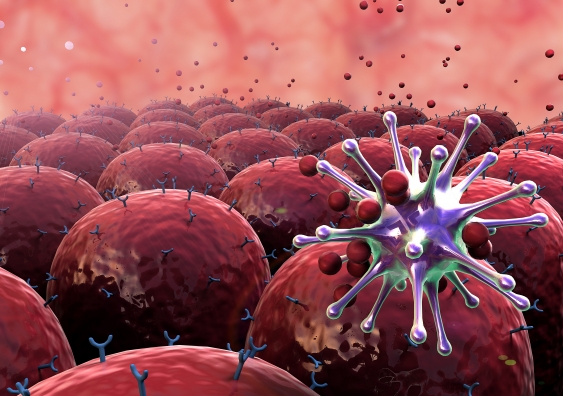
UNSW scientists have discovered how human immune receptors become activated in the presence of harmful substances, paving the way for new technologies to fight against deadly diseases.