Explainer: what is nanomedicine and how can it improve childhood cancer treatment?
The emerging field of nanomedicine offers hope for better children’s cancer treatment that will have fewer side effects and improve quality of life for survivors.
The emerging field of nanomedicine offers hope for better children’s cancer treatment that will have fewer side effects and improve quality of life for survivors.
A recent US study of people treated for cancer as children from the 1970s to 1999 showed that although survival rates have improved over the years, the quality of life for survivors is low. It also showed this was worse for those who were treated in the 1990s.
About 70% of childhood cancer survivors experience side effects from their treatment, including secondary cancers. And as survival rates improve, the worldwide population of childhood cancer survivors is growing.
Side effects cause stress for survivors and families and increase demand on health systems. But an emerging area of medicine, nanomedicine, offers hope for better children’s cancer treatment that will have fewer side effects and improve quality of life for survivors.
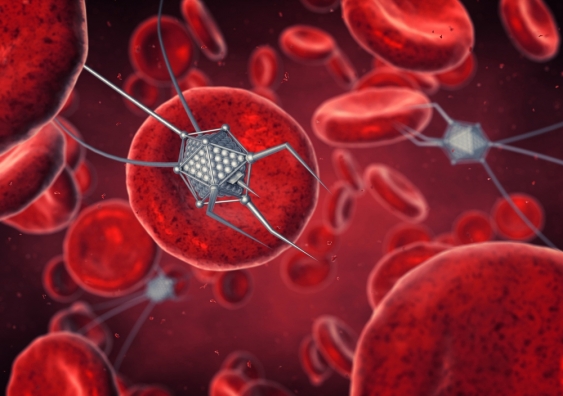
Nanomedicine is the application of nanomaterials, or nanoparticles, to medicine. Nanoparticles are a form of transport for drugs and can go places drugs wouldn’t be able to go on their own.
Nano means tiny. A nanometre (nm) is one-billionth of a metre. Nanoparticles used for drug delivery are usually in the 20 to 100 nanometre range, although this can vary depending on the design of the nanoparticle.
Nanoparticles can be engineered and designed to package and transport drugs directly to where they’re needed. This targeted approach means the drugs cause most harm in the particular, and intended, area of the tumour they are delivered to. This minimises collateral damage to surrounding healthy tissues, and therefore the side effects.

The first cancer nanomedicine approved by the US Food and Drug Administration was Doxil. Since 1995, it has been used to treat adult cancers including ovarian cancer, multiple myeloma and Kaposi’s sarcoma (a rare cancer that often affects people with immune deficiency such as HIV and AIDS).
Currently, there is a stream of new nanomedicine treatments for adult cancers in clinical trials (trials in humans), or on the market. But only a limited number of these have been approved for children’s cancers, although this is arguably where nanomedicine’s strengths could have the most benefit.
The nanoparticle drug-delivery systems can work in different ways. Along with carrying the drug for delivery, nanoparticles can be engineered to carry specific compounds that will let them bind, or attach, to molecules on tumour cells. Once attached, they can safely deliver the drug to the specific tumour site.
Nanoparticles can also help with drug solubility. For a drug to work, it must be able to enter the bloodstream, which means it needs to be soluble. For example, the cancer drug paclitaxel (Taxol) is insoluble so has to be dissolved in a delivery agent to get into the blood. But this agent can cause allergic reactions in patients.
To overcome these issues, chemists have developed a nanoparticle out of the naturally occurring protein albumin. It carries the paclitaxel and makes it soluble but without the allergic reactions.
Tumours commonly have disordered and leaky blood vessels sprouting through and off them. These vessels allow chemotherapy drugs to readily enter the tumour, but because chemotherapy molecules are so small, they also diffuse through the vessels and out of the tumour, attacking surrounding tissues. Nanoparticles are larger molecules that get trapped inside the tumour, where they do all the damage.
Once they have delivered their drug cargo to cells, nanoparticles can be designed to break down into harmless byproducts. This is particularly important for children who are still developing.
Nanoparticles vary in characteristics like shape and size. Researchers need to match the right nanoparticle to the drug it’s to deliver and the particular tumour.
An array of nanoparticle structures are currently being engineered. One example of an interesting structure is the shape of a DNA origami. Because DNA is a biological material, nanoparticles engineered into DNA origami shapes won’t be seen as foreign by the immune system. So these can transport a drug to diseased cells while evading the body’s immune system, therefore lessening the side effects of drugs.
Another example of nanomedicine structures are polymeric nanocarriers. We have recently identified a gene that promotes the growth of tumours, cancer spread and resistance to chemotherapy in pancreatic cancers.
We used a nanomedicine called a polymeric nanocarrier and combined it with a drug that silences the cancer gene. We packaged this up to form a nanomedicine and delivered the drugs into the tumour.
These nanomedicines reduced the expression of the cancer gene, blocked tumour growth and reduced the spread of pancreatic cancer. But we also showed that polymeric nanocarriers can be combined in the lab with other gene-silencing drugs. This means the method can be used for a range of other gene-based cancers.

In standard treatment for children’s cancer, chemotherapy drugs are often prescribed at the maximum tolerable dose for a child’s age or size, based on adult dosages. But children aren’t small adults. The processes underlying children’s growth and development might lead to a different effect and response to a chemotherapy drug not seen in adults.
Also, if a child becomes resistant to a drug and they’re on the maximum tolerable dose, there’s no scope to increase it without toxic side effects. By packaging up drugs and moving them through the body directly to diseased cells to reduce collateral damage, in theory, nanomedicine allows higher doses of drugs to be used.
Nanomedicine has great potential to safely treat children’s cancer. However, it is currently stymied by too little research. About two-thirds of research attention in nanomedicine therapeutics, of more 250 nanomedicine products, is focused on cancer. Yet this isn’t translating into new cancer treatments for children coming to market.
But we are making progress. Our work is exploring the design of nanoparticles to deliver gene-silencing drugs to treat the most common brain cancer in children – medulloblastoma.
We’re also working on nanomedicines for other significant childhood cancers. These include drug-refractory acute lymphoblastic leukaemia, the most common childhood cancer, and neuroblastoma, the cancer that claims more lives of those under five than any other.
Maria Kavallaris, Professor, Children's Cancer Institute; Joshua McCarroll, Project Leader, Children's Cancer Institute and Senior Lecturer, Medicine, UNSW; Thomas P Davis, ARC Laureate Fellow, Monash University.
This article was first published on The Conversation. Read the original article.