New South Wales on a knife edge as cumulative coronavirus case numbers spiral into the 'red zone'
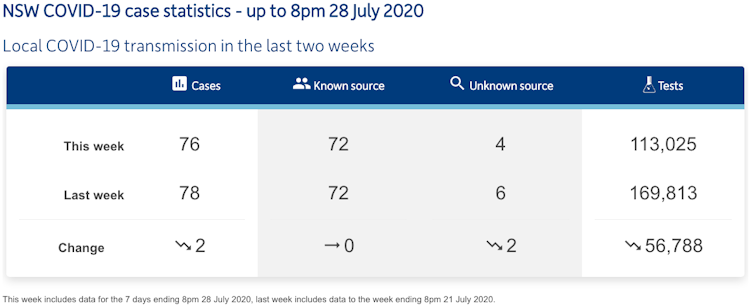
Analysis suggests when COVID-19 cases reach 100 over 14 days, an outbreak gets very difficult to control — as we saw in Victoria. Over the last fortnight, NSW has recorded at least 154 new cases.