Globally, common lung diseases including acute respiratory infections (ARIs) and asthma are the most common causes of morbidity and mortality in children. Our internationally recognised program of research aims to determine the modifiable factors associated with poor health outcomes in children and translate that knowledge into prevention of CoLD.
Asthma care from home
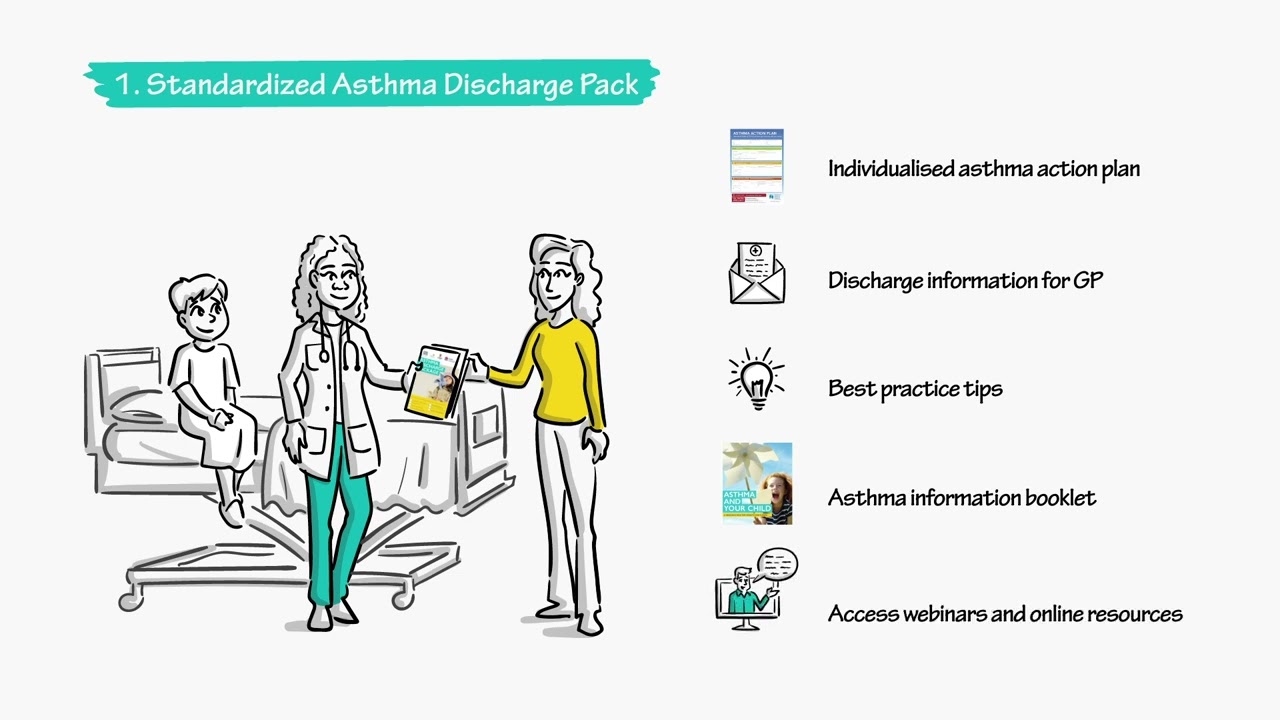
We have developed an integrated model of asthma care for children with the aim to standardise asthma care, reduce avoidable asthma hospital presentations and improve quality of life of children leaving with asthma. This model of asthma care is being rolled out across multiple rural and metropolitan settings across New South Wales through funding we received from New South Wales Health, Asthma Australia and Sydney Children’s Hospital foundation. This is an evidence-based model and can be adopted in different settings.
Our goals
- Prevention of CoLD:
- Estimating burden of disease including hospitalisation, mortality, and economic burden.
- Investigate risk factors associated with high burden of disease.
- Establish the link between acute respiratory infections and chronic lung diseases.
- Control and management of CoLD:
- Improving quality: Standardisation of clinical care.
- Improving access to care: Technology-enabled models of care.
- Improving equity to care: Evaluating impact of public health interventions in reducing burden of disease.
- Evaluating novel models for care for vulnerable children.
Research Strengths
Designing and establishing surveillance, application and analysis of record-linked administrative health data ("big data"); design and conduct of randomised controlled trials, clinical surveys, diagnostic studies and longitudinal studies, systematic reviews and meta-analyses and health service research.
Our results
Our program of research has demonstrated:
- Globally respiratory infections associated with respiratory syncytial virus (RSV) and influenza virus are the leading causes of morbidity in children aged <5 year.
- COVID-19 is associated with mild respiratory disease in children aged <5 years.
- Burden of respiratory infections is double in Aboriginal compared to non-Aboriginal children.
- The 13v pneumococcal conjugate vaccine does not provide optimal protection against invasive pneumococcal pneumonia in Australian children.
- Children with asthma were not at greater risk of COVID-19 severity at any stage of the pandemic regardless of the SARS-CoV-2 variants/subvariants.
- There is wide variation in clinical management of CoLD of childhood .
- Comprehensive multicomponent integrated model of care can reduce healthcare burden and improve quality of life associated with CoLD in children.
Ongoing projects:
- Monitoring the impact of severe RSV-associated acute lower respiratory infection (ALRI) compared to non-RSV ALRIs in children aged<2 years: a multi-site prospective observational study: Funded by MSD Global.
- Asthma care from home: Implementation and evaluation of a technology-enabled flexible model of care for children in rural New South Wales: Funded by NSW MoH Translational Research Grant Scheme (Round 6)
- Comprehensive Community-based Care Coordination for Management of Paediatric Asthma (CoMPAs): Funded by Asthma Australia and Sydney Children’s Hospitals Foundation
- Asthma and respiratory infection and its impact on healthcare utilisation: Funded by Rotary Club philanthropy and Sydney Children’s Hospital
- Long-term impact of chronic lung diseases in children: Funded by UNSW Philanthropy.
- Improving diagnosis and management of CoLD using novel machine learning technologies.