On International Overdose Awareness Day on Monday, 31 August, it is important to raise awareness and acknowledge the grief felt by families and friends of those who have died or sustained a permanent injury as a result of overdose.
NDARC research shows that there were 1,740 drug-induced deaths in Australia in 2018. This equates to nearly five drug-induced deaths per day. Most of these deaths were accidental.
While these numbers reflect lives lost, many more people are impacted by overdose through non-fatal events. It is estimated that 3.2 (1.8–5.2) million people who inject drugs globally have experienced at least one non-fatal overdose in the previous year.
In Australia specifically, NDARC research has shown that 20.5 per cent and 41.5 per cent of people surveyed who inject drugs had experienced a non-fatal event in the previous 12 months and lifetime, respectively. This is a concerning picture, as non-fatal overdose is a major risk factor for both subsequent fatal overdose and morbidity.
These accidental overdoses are preventable. Interventions such as opioid agonist treatment have a demonstrable positive effect in reducing overdose risk. Importantly though, people need to have access to naloxone to reverse opioid overdose.
What is naloxone?
Naloxone (also known as Narcan®) is an opioid antagonist that is a safe and effective agent for reversing the effects of opioids, including pharmaceutical opioids (e.g. methadone, codeine, fentanyl and morphine) and illicit opioids (e.g. heroin).
Naloxone ‘clears’ the opioid receptors temporarily, overriding the effects of any opioids that have been taken. This allows a person to breathe again, reversing the effects of an overdose. Naloxone can be administered as an intramuscular injection or nasal spray.
Initiatives such as the rescheduling of naloxone in 2016, allowing supply over the counter without prescription, and the advent of jurisdictional take home naloxone (THN) programs have been implemented with the intention to increase the uptake and deployment of this medication.
More recent changes, such as listing the intranasal spray formulation (Nyxoid) on the Pharmaceutical Benefits Scheme, and a Commonwealth-funded pilot providing free take-home naloxone in NSW, SA and WA, have been introduced in an attempt to overcome some of the previously noted barriers to naloxone uptake
Are people using naloxone?
NDARC research suggests that people who inject drugs are increasingly aware of, accessing, and using take-home naloxone to reverse overdoses.
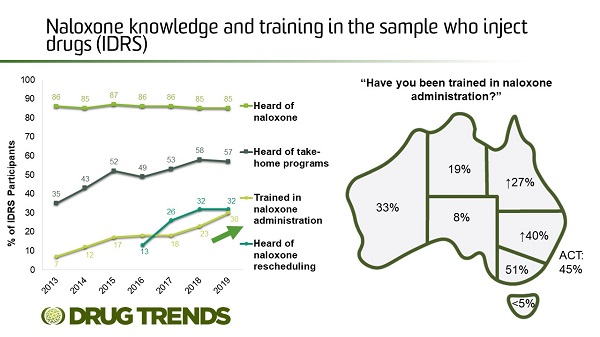
Of a sample of 902 Australians who regularly inject drugs interviewed in 2019, most had heard of naloxone, three-in-five had heard of take-home naloxone training programs, and one-in-three were trained in naloxone administration. However, the latter varied considerably across jurisdictional samples, ranging from less than five per cent of participants in Hobart, Tasmania, to 51 per cent of participants in Melbourne, Victoria. Some people cite issues around availability and costs of naloxone.
Also, one-in-twenty participants reported being resuscitated with naloxone by someone who had participated in training programs, and half of those who had participated in training programs reported resuscitating someone.
This research shows that people are aware of naloxone, and are using training they have received to resuscitate others experiencing non-fatal overdose.
There is also a need to promote naloxone amongst other groups at risk of experiencing overdose (e.g., people who use pharmaceutical opioids for chronic non-cancer pain), and to other people who may be at risk of witnessing overdose.
Naloxone for people leaving prison
In a recent paper, ‘Feasibility and acceptability of take‐home naloxone for people released from prison in New South Wales, Australia’ it was found that among people with a history of opioid use who had recently left prison, there was very high awareness of the elevated risk of overdose following release from prison (95 per cent) and the potential for naloxone to reverse an opioid overdose (97 per cent) (Moradmand-Badie et al 2020).
As proactively accessing naloxone is a low priority for patients, naloxone supply at release may be more effective than programs that refer releasees to local pharmacies, but developing a sustainable supply model requires consideration of several barriers (Moradmand-Badie et al 2020).
Expanding awareness and use
Anyone can access naloxone over-the-counter from a pharmacy. There’s strong evidence to suggest that naloxone can be used safely by people who are not medical professionals. It’s important that people are trained to recognise signs of an overdose, and to administer naloxone where they may be at risk of witnessing an overdose. To find locations where naloxone can be purchased, click here. To find out how to identify and respond to an opioid overdose, go here.
Further, much attention to date has concentrated on people who use non-prescribed opioids. The Australian Government’s Take-Home Naloxone Pilot is partly concentrated on expanding naloxone access to other groups who may be at risk of experiencing and witnessing overdose, including people who are prescribed pharmaceutical opioids for non-cancer pain.
Distribution of more acceptable formulations (such as intranasal sprays) may also increase the use of naloxone to prevent opioid overdose deaths.
FREE Webinar - ‘How to identity and respond to an opioid overdose’
Rosie Gilliver from Kirketon Road Centre presented at the 2020 NDARC Webinar Series, providing information on how to identify and respond to an opioid overdose, as well as how to administer Nyxoid Naloxone nasal spray in the event of overdose.
International Overdose Awareness Day
International Overdose Awareness Day aims to raise awareness of overdose and reduce the stigma of a drug-related death. It is also an opportunity to stimulate discussion about evidence-based overdose prevention and drug policy. Click here to read more about International Overdose Awareness Day.
If you think someone is experiencing an overdose, please call Triple Zero (000).
For free and confidential advice about alcohol and other drugs call the National Alcohol and Other Drug Hotline on 1800 250 015.
References
Colledge, S. Peacock, A. Leung, J. Larney, S. Grebely, J. Hickman, M. Cunningham, E. Trickey, A. Stone, J. Vickerman, P. Degenhardt, L. The prevalence of non-fatal overdose among people who inject drugs: A multi-stage systematic review and meta-analysis. International Journal of Drug Policy. November, 2019. doi.org/10.1016/j.drugpo.2019.07.030
Dwyer, R., Olsen, A. Fowlie, C. Gough, C. van Beek, I., Jauncey, M., Lintzeris, N., Oh, G., Dicka, J., Fry, C.CL., Hayllar, J., Lenton, S. An overview of take-home naloxone programs in Australia. Drug & Alcohol Review. 2018; 37(4): 440-449
Lenton SR, Dietze PM, Jauncey M. Australia reschedules naloxone for opioid overdose. The Medical Journal of Australia. 2016;204(4):146-7
Man, N., Chrzanowska, A., Dobbins, T., Degenhardt, L. & Peacock, A. (2019). Trends in drug-induced deaths in Australia, 1997-2018. Drug Trends Bulletin Series. Sydney: National Drug and Alcohol Research Centre, UNSW Sydney.
Moradmand-Badie, B. Tran, L. Oikarainen, N. Degenhardt, L. Nielsen, S, Roberts, J. Ward, S. Bowman, J. Larney, S. Feasibility and acceptability of take‐home naloxone for people released from prison in New South Wales, Australia. Drug and Alcohol Review. August 2020. doi.org/10.1111/dar.13144
Peacock, A., Uporova, J., Karlsson, A., Gibbs, D., Swanton, R., Kelly, G., Price, O., Bruno, R., Dietze, P., Lenton, S., Salom, C., Degenhardt, L., & Farrell, M. (2019). Australian Drug Trends 2019: Key Findings from the National Illicit Drug Reporting System (IDRS) Interviews. Sydney: National Drug and Alcohol Research Centre, UNSW Sydney.
Salom, C. Daly, C. Juckel, J. Morris, L. (2020). Trends in awareness, uptake and deployment of naloxone among a sample of people who inject drugs in Australia. Drug Trends Bulletin Series. Sydney: The National Drug and Alcohol Research Centre, UNSW Sydney.
Sharman, C. & Bruno, R. (2019). Trends in Naloxone Use Among a Sample of People Who Inject Drugs in Tasmania. Drug Trends Bulletin Series. Sydney: National Drug and Alcohol Research Centre, University of New South Wales.
Sordo, L., Barrio, G., Bravo, M., Indave, B., Degenhardt, L., Wiessing, L., Ferri, M., Pastor-Barriuso, R. (2017). Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ, 357, doi: 10.1136/bmj.j1550
Of a sample of 902 Australians who regularly inject drugs interviewed in 2019, most had heard of naloxone, three-in-five had heard of take-home naloxone training programs, and one-in-three were trained in naloxone administration. However, the latter varied considerably across jurisdictional samples, ranging from less than five per cent of participants in Hobart, Tasmania, to 51 per cent of participants in Melbourne, Victoria. Some people cite issues around availability and costs of naloxone.
Also, one-in-twenty participants reported being resuscitated with naloxone by someone who had participated in training programs, and half of those who had participated in training programs reported resuscitating someone.
This research shows that people are aware of naloxone, and are using training they have received to resuscitate others experiencing non-fatal overdose.
There is also a need to promote naloxone amongst other groups at risk of experiencing overdose (e.g., people who use pharmaceutical opioids for chronic non-cancer pain), and to other people who may be at risk of witnessing overdose.
Naloxone for people leaving prison
In a recent paper, ‘Feasibility and acceptability of take‐home naloxone for people released from prison in New South Wales, Australia’ it was found that among people with a history of opioid use who had recently left prison, there was very high awareness of the elevated risk of overdose following release from prison (95 per cent) and the potential for naloxone to reverse an opioid overdose (97 per cent) (Moradmand-Badie et al 2020).
As proactively accessing naloxone is a low priority for patients, naloxone supply at release may be more effective than programs that refer releasees to local pharmacies, but developing a sustainable supply model requires consideration of several barriers (Moradmand-Badie et al 2020).
Expanding awareness and use
Anyone can access naloxone over-the-counter from a pharmacy. There’s strong evidence to suggest that naloxone can be used safely by people who are not medical professionals. It’s important that people are trained to recognise signs of an overdose, and to administer naloxone where they may be at risk of witnessing an overdose. To find locations where naloxone can be purchased, click here. To find out how to identify and respond to an opioid overdose, go here.
Further, much attention to date has concentrated on people who use non-prescribed opioids. The Australian Government’s Take-Home Naloxone Pilot is partly concentrated on expanding naloxone access to other groups who may be at risk of experiencing and witnessing overdose, including people who are prescribed pharmaceutical opioids for non-cancer pain.
Distribution of more acceptable formulations (such as intranasal sprays) may also increase the use of naloxone to prevent opioid overdose deaths.
FREE Webinar - ‘How to identity and respond to an opioid overdose’
Rosie Gilliver from Kirketon Road Centre presented at the 2020 NDARC Webinar Series, providing information on how to identify and respond to an opioid overdose, as well as how to administer Nyxoid Naloxone nasal spray in the event of overdose.
International Overdose Awareness Day
International Overdose Awareness Day aims to raise awareness of overdose and reduce the stigma of a drug-related death. It is also an opportunity to stimulate discussion about evidence-based overdose prevention and drug policy. Click here to read more about International Overdose Awareness Day.
If you think someone is experiencing an overdose, please call Triple Zero (000).
For free and confidential advice about alcohol and other drugs call the National Alcohol and Other Drug Hotline on 1800 250 015.
References
Colledge, S. Peacock, A. Leung, J. Larney, S. Grebely, J. Hickman, M. Cunningham, E. Trickey, A. Stone, J. Vickerman, P. Degenhardt, L. The prevalence of non-fatal overdose among people who inject drugs: A multi-stage systematic review and meta-analysis. International Journal of Drug Policy. November, 2019. doi.org/10.1016/j.drugpo.2019.07.030
Dwyer, R., Olsen, A. Fowlie, C. Gough, C. van Beek, I., Jauncey, M., Lintzeris, N., Oh, G., Dicka, J., Fry, C.CL., Hayllar, J., Lenton, S. An overview of take-home naloxone programs in Australia. Drug & Alcohol Review. 2018; 37(4): 440-449
Lenton SR, Dietze PM, Jauncey M. Australia reschedules naloxone for opioid overdose. The Medical Journal of Australia. 2016;204(4):146-7
Man, N., Chrzanowska, A., Dobbins, T., Degenhardt, L. & Peacock, A. (2019). Trends in drug-induced deaths in Australia, 1997-2018. Drug Trends Bulletin Series. Sydney: National Drug and Alcohol Research Centre, UNSW Sydney.
Moradmand-Badie, B. Tran, L. Oikarainen, N. Degenhardt, L. Nielsen, S, Roberts, J. Ward, S. Bowman, J. Larney, S. Feasibility and acceptability of take‐home naloxone for people released from prison in New South Wales, Australia. Drug and Alcohol Review. August 2020. doi.org/10.1111/dar.13144
Peacock, A., Uporova, J., Karlsson, A., Gibbs, D., Swanton, R., Kelly, G., Price, O., Bruno, R., Dietze, P., Lenton, S., Salom, C., Degenhardt, L., & Farrell, M. (2019). Australian Drug Trends 2019: Key Findings from the National Illicit Drug Reporting System (IDRS) Interviews. Sydney: National Drug and Alcohol Research Centre, UNSW Sydney.
Salom, C. Daly, C. Juckel, J. Morris, L. (2020). Trends in awareness, uptake and deployment of naloxone among a sample of people who inject drugs in Australia. Drug Trends Bulletin Series. Sydney: The National Drug and Alcohol Research Centre, UNSW Sydney.
Sharman, C. & Bruno, R. (2019). Trends in Naloxone Use Among a Sample of People Who Inject Drugs in Tasmania. Drug Trends Bulletin Series. Sydney: National Drug and Alcohol Research Centre, University of New South Wales.
Sordo, L., Barrio, G., Bravo, M., Indave, B., Degenhardt, L., Wiessing, L., Ferri, M., Pastor-Barriuso, R. (2017). Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ, 357, doi: 10.1136/bmj.j1550
