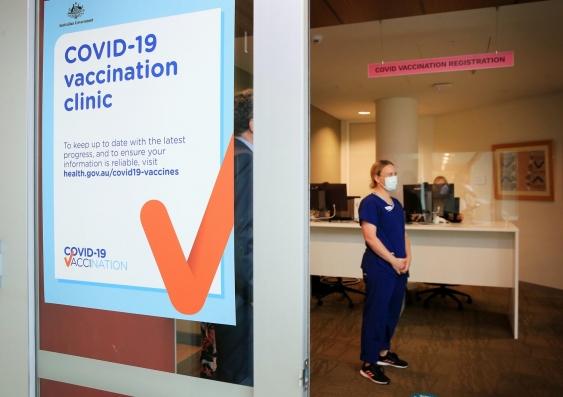
How can governments communicate with multicultural Australians about COVID vaccines?
Our new research found gaps in COVID information available to culturally and linguistically diverse communities. But there are ways we can improve — because community ownership is crucial.