Rapid lab analysis informs global guidelines on COVID-19 vaccination and treatment
Researchers from the Kirby Institute have developed a world-first method for rapid isolation and characterisation of COVID-19 variants.
Researchers from the Kirby Institute have developed a world-first method for rapid isolation and characterisation of COVID-19 variants.
Kirby Institute researchers at UNSW Sydney have developed a methodology that speeds up the process for isolating and characterising the risks posed by COVID-19 variants of concern. The methodology, which has been shared with the global scientific community through publication in Nature Microbiology today, is highly cost-effective, automated, and can be used to measure the effectiveness of therapeutics and scaled to test thousands of samples.
The methodology, called R-20, was used to analyse all major circulating viral variants in 2021 that were identified from patients in hotel quarantine. At the end of 2021, it was applied to Australia’s first Omicron samples. The researchers found that the vaccine-induced antibody response to Omicron was 15-20-fold weaker than to the original SARS-CoV-2 strain.
The rapid analysis included details of how well the variant evades antibodies and how resilient it is. The results have been cited in Centers for Disease Control and Prevention (CDC) guidelines, World Health Organization (WHO) technical reports and by the Australian Technical Advisory group on Immunisation (ATAGI) regarding the use of booster vaccinations.
“What makes our R-20 approach unique is its speed and accuracy,” says Associate Professor Turville who developed the methodology. “The best way to quickly understand how a virus works is to genetically develop a cell with receptors that the virus likes. R-20 uses 'supercharged' cells that allow the virus to replicate four times faster than through any other techniques currently published in the scientific literature.”
The Kirby Institute team took lessons learned from HIV to develop cells with receptors that viruses ‘like’. They looked at hundreds of different cells to identify ones that would allow the virus to replicate as quickly and effectively as possible. A/Prof. Turville calls these cells the ‘canaries in the coal mine’ – because they effectively die in the process of telling his team what each variant is up to. They also allow his team to capture variants of the virus quicker than any other cell culture method, with sensitivities approaching that of a PCR swab test.
Read more: 'Supercharged' cells help scientists analyse SARS-CoV-2 variants faster
“These cells are an incredible asset to the Australian response to COVID-19, but the other crucial part of this process is getting rapid access to samples as they are identified,” says A/Prof. Turville. “This is where our collaborative relationships with clinical and diagnostic partners have been crucial. With the support of clinical partners, we were one of only a few labs globally that had access to all variants of concern, which is particularly impressive considering Australian borders were closed for most of 2021.”
Professor Anthony Kelleher, Director of the Kirby Institute and co-author on the research says, “These deeply collaborative clinical-research partnerships facilitated high-quality, rapid and translational research that we are seeing inform clinical guidelines across the globe.”
Using R-20, the researchers look at viral properties of variants to understand how sick the virus is likely to make the population, as well as how evasive it is to existing vaccines and treatments. Identifying this quickly is crucial to inform public health policies such as vaccination strategies, which therapeutics will still work and advice on mask use to mitigate spread of variants to vulnerable populations such as the elderly.
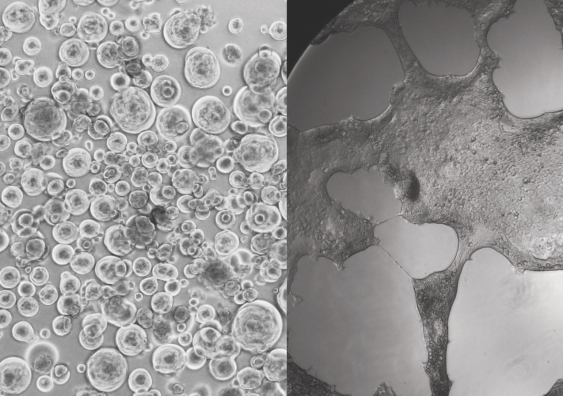
“Omicron looked very different under the microscope to all other variants we’d seen before,” says A/Prof. Turville. “It was the most evasive and transmissible variant observed at the time. The other issue is that it had changed the way it enters our bodies. It is using a pathway that diverges from all other variants.
“This is why a lot of people contracted Omicron even though they were two-dose or even three-dose vaccinated,” says A/Prof. Turville. "Fortunately though, while vaccination doesn’t prevent most people contracting Omicron, in most cases it does prevent the disease from becoming severe. Vaccines are doing the most important job well, but we need to think carefully about how we can modify them to reduce spread better in the Omicron era.”
The Kirby Institute team were also the first globally to measure the immune response to Omicron using a pooled clinical grade hyper-immune IgG (HIgG) product, which is derived from plasma from thousands of donors who have developed antibodies through natural infection and/or vaccination.
They found a 16-fold reduction in antibodies from concentrate batches containing a mixture of vaccinated, convalescent and non-convalescent US donors as well as a batch produced in 2020 from convalescent US/EU donors only.

Members of the Kirby Institute research team. Photo: Richard Freeman/UNSW.
“This product is very useful as it is a good indicator of immunity to COVID-19 in the broader global community and includes plasma from thousands of people who have either recovered from pre-Omicron variants and/or have had two doses of the vaccine,” says Prof. Kelleher. “Testing against thousands of donors that are pooled gives a great population snapshot of circulating antibodies at that point in time and what a threat an emerging variant is to infecting a population.
“It’s another example of the strength of collaborative relationships in Australia, that is seeded from clinical-research partnerships and then branches out with partnerships with industry.”
In collaboration with teams at the Garvan Institute headed by Professor Daniel Christ, the team also tested all clinically available monoclonal antibody treatments, which are proteins produced in the laboratory that mimic human antibodies, stimulating the body’s immune response. While many did not work against Omicron, the team did observe that those developed by AstraZeneca (Evusheld) and also GSK (Sotrovimab) offered a sufficient immune response against the virus.
During Australia’s first Omicron wave, researchers were able to confirm in real-time that the available stockpile of Sotrovimab was still effective.