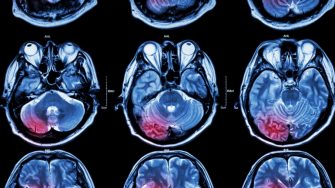
Linking Kidney Function Changes to Recurrent Stroke and Dementia
In a groundbreaking analysis of the Perindopril Protection Against Recurrent Stroke Study (PROGRESS), researchers have delved into the effects of fluctuating kidney function on cardiovascular outcomes.