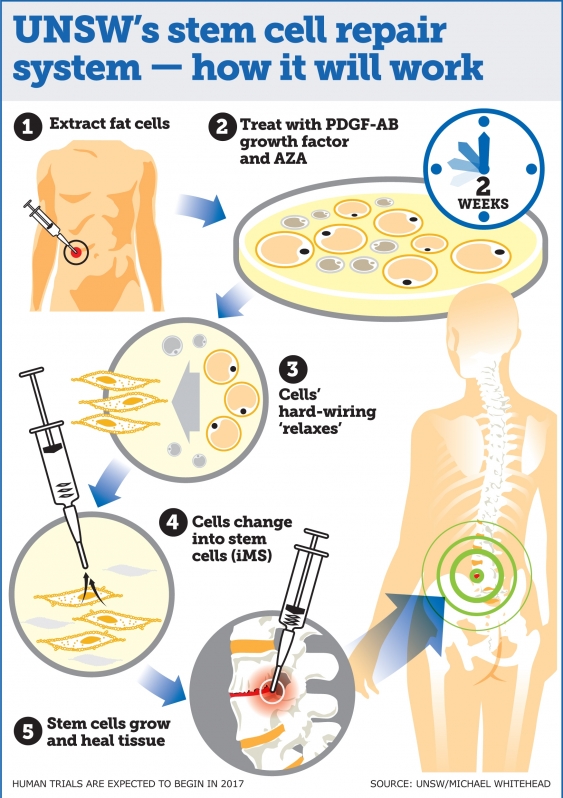
Medical scientists develop ‘game changing’ stem cell repair system
Stem cell therapies capable of regenerating any human tissue damaged by injury, disease or ageing could be available within a few years, following breakthrough research led by UNSW researchers.