Decision-making mechanisms go awry in OCD brains: study
The research sheds light on the biological basis of obsessive-compulsive disorder (OCD).
The research sheds light on the biological basis of obsessive-compulsive disorder (OCD).

Maddie Massy
UNSW Medicine & Health
+61 2 9348 1936
m.massywestropp@unsw.edu.au
A new study from UNSW Sydney shows that teenagers with OCD experience deficits in decision making and behavioural control. This is linked to abnormal activity in an area of the brain called the orbitofrontal cortex (OFC). The research is published this week in Biological Psychiatry Global Open Science.
“OCD is highly prevalent, affecting more than 750,000 Australians. People with OCD get stuck in loops of unwanted thoughts and behaviours,” says first author Dr Iain Perkes, Senior Lecturer at UNSW Medicine & Health and child and adolescent psychiatrist in Sydney Children’s Hospitals Network.
The researchers aimed to better understand the biological basis of OCD, which could lead to the development of new treatments. They focused on adolescents in the study, which is important given that OCD typically develops in childhood or adolescence.
“These repetitive actions, obsessions and compulsions aren’t completely under the control of someone with OCD. Otherwise, they would simply choose not to do them,” Dr Perkes says.
“So, there was good reason to think that those decision-making mechanisms in the brain go awry in the case of OCD.”
This study builds upon previous research by Scientia Professor Bernard Balleine from UNSW Science, isolating the brain processes behind decision making.
Prof. Balleine, who is the senior author of this paper, leads the UNSW Decision Neuroscience Lab. The lab has conducted an extensive research program involving behavioural experiments in rats. This is combined with studies of the brain to understand which areas of the brain activate, and how they communicate, to contribute to decision making.
Through collaboration with clinical researchers like Dr Perkes, this research can now be translated to humans.
The study involved 21 healthy adolescents and 20 adolescents with OCD. Participants were given decision-making tasks to gain small food rewards. They did these tasks inside a magnetic resonance imaging (MRI) scanner, which showed blood flow in their brains associated with brain activity.

During the experiment, participants completed decision-making tasks, for example playing a computer game where they tilted a vending machine in different directions to earn different food rewards. Sometimes the food rewards were ‘devalued’, with the participants being shown a video of insects crawling over the food. Image: Supplied.
Participants were tested in terms of their ability to make decisions based on environmental cues, in exchange for food rewards. For example, in one of the activities they played a computer game where they learned to tilt a vending machine in different directions, which corresponded to different snacks.
“We make decisions every day based on environmental cues – for example, stop signals and go signals that we see at traffic lights. These cues allow us to predict the circumstances around us,” Dr Perkes says.
Before one of the decision-making tasks, the ‘value’ of the food rewards was reduced; the participants were shown a video of insects crawling over the food, making it less desirable.
“We wanted to see how changing the value of the reward would change the choice of action for healthy young people, versus young people with OCD,” Dr Perkes says.
Compared to the control group, adolescents with OCD struggled to make choices and control their behaviour to gain food rewards. In addition, when the value of the food rewards was reduced, this had little influence on their behaviour during the tasks.
“People with OCD experience difficulties using reward signals to guide their choices in an adaptive way. Those behavioural difficulties are associated with changes in the brain,” Dr Perkes says.
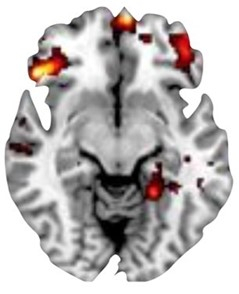
MRI scan showing hyperactivity in the OFC during decision-making, which is linked to OCD symptom severity. Image: Supplied.
The MRI scans showed different patterns of activity in the brain for adolescents with OCD, compared to healthy adolescents. The differences were particularly strong in the OFC, a region of the brain responsible for decision-making, behavioural control and other cognitive functions.
In participants with OCD, specific areas of the OFC were hyperactive and others were hypoactive during the two decision-making tasks. These findings are consistent with previous research in rats, providing evidence of the specific OFC areas responsible for these psychological functions.
The researchers also found that for adolescents with OCD, hyperactivity of the OFC during the experiments was linked to the severity of OCD symptoms. This further supports the connection between decision-making performance and the disorder.
“This is strong evidence that these mechanisms have a core role in the development of OCD,” Dr Perkes says.
This study provides more support for the biological basis for OCD. According to Dr Perkes, people with OCD are sometimes invalidated by others when they struggle with unwanted thoughts and behaviours.
“As we understand the biological reality and underpinnings of mental health conditions like OCD, it helps to reduce stigma,” Dr Perkes says.
“It shifts the dialogue from ‘Just pull your socks up, work harder’ to ‘There are changes in the brain, that’s a real health condition.’”
A better understanding of the root causes and important brain regions for OCD also takes us further towards developing better treatments. For example, these findings could contribute to more targeted transcranial magnetic stimulation, which is sometimes used to target nerve cells in the brain to treat OCD. Also, knowledge about OCD decision-making processes could lead to more tailored behavioural therapies.
“We know that for one third of people living with OCD, they don’t respond to first-line treatments,” Dr Perkes says.
“There is a real need to continue discovering new and better treatment paradigms.”