It's not all in their DNA: cancer cells with the same genome can behave differently
Scientists have tracked and analysed cancer cell behaviour with a novel cellular ‘barcoding technology’.
Scientists have tracked and analysed cancer cell behaviour with a novel cellular ‘barcoding technology’.
For the first time, research has shown cancer cells with the same genetic blueprint won't necessarily behave in the same way, with serious implications for how we target them.
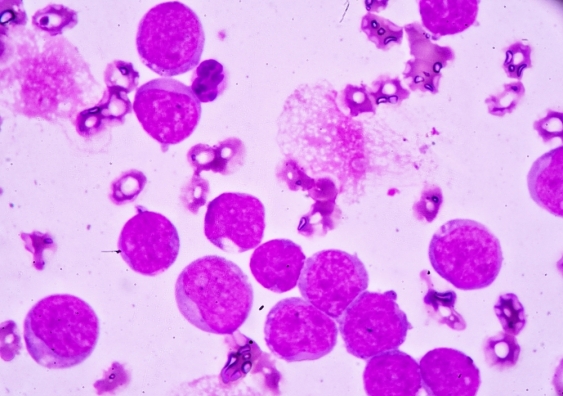
A Peter Mac-led study involving a UNSW scientist demonstrating these non-genetic changes in acute myeloid leukaemia cells was published today in Nature.
Joint first author Dr Katie Fennell says: “We developed a novel cellular barcoding technology that can track individual cancer cells over time and identify patterns that lead to different cell behaviour – even when the underlying genome is the same.”
This barcoding technology (dubbed SPLINTR, which stands for Single-cell Profiling and LINeage TRacing) helps the researchers to identify the unique genes expressed in each leukaemia cell, and monitor how this influences the cancer's behaviour over time. They can then observe which acute myeloid leukaemia cells are most likely to form cancerous tumours.
UNSW scientist and co-author Dr Emily Wong, who is based at the Victor Chang Cardiac Research Institute, says the fact that regulatory changes are key contributors to disease in the absence of genetic mutations is only starting to be widely recognized.
“The Dawson Lab has developed an exciting method to track the regulatory genome of individual cancer cells over time. We are pleased to be able to contribute our computational analyses to this major advance.”
While this study is in acute myeloid leukaemia, the technology can be applied to many different cancers, presenting an opportunity to understand why some tumour cells survive drug treatment or relapse in specific organs.
Drug resistance and tumour recurrence are major barriers to the successful treatment of cancer, and often arise from rare populations of tumour cells, which can be difficult to monitor in the clinic.
“Our study highlights the power of using SPLINTR to not only identify these rare tumour subpopulations, but also to find novel therapeutic targets and/or biomarkers to monitor them clinically,” says joint first author Dr Dane Vassiliadis.
“This work challenges the dogma that precision medicine is just about finding new genetic mutations,” says senior author on the paper Professor Mark Dawson.
While all precision medicine aims to tailor treatment to the unique features present in a patient’s cancer, thus far these approaches have exclusively focused on the unique DNA mutations present.
However, recent studies show that up to 40 per cent of tumours that relapse after initially responding to treatment show no evidence of new gene mutations in the cancer cells to account for this therapy resistance.
This study highlights the importance of broadening the ambition of precision medicine beyond just surveying a patient’s DNA mutations.
“This is only one side of the coin. We urgently need to understand and develop treatments to also counter the non-genetic factors that influence cancer cell behaviour,” says Dr Vassiliadis.
The research was led by Peter Mac and done in collaboration with academic partners at UNSW, the Victor Chang Cardiac Research Institute, The University of Melbourne, and WEHI.