New 3D stretchable electronics can advance organ-on-chip technology
Flexible electronic nanomembranes show promise for revolutionary organ-on-chip technologies, potentially reducing the need for animal testing in medical research.
Flexible electronic nanomembranes show promise for revolutionary organ-on-chip technologies, potentially reducing the need for animal testing in medical research.
Engineers from UNSW Sydney have discovered a way to create flexible electronic systems on ultra-thin skin-like materials.
The development allows entire stretchable 3D structures to operate like a semiconductor and could help significantly reduce the need for animal testing by making so-called organ-on-chip technology more effective.
Down the track, the technology could also be used in wearable health monitoring systems or implantable biomedical applications, such as a system to alert people with epilepsy of an imminent seizure.
The research team, led by Dr Hoang-Phuong Phan from UNSW’s School of Mechanical and Manufacturing Engineering, have published their findings in the Advanced Functional Materials journal.
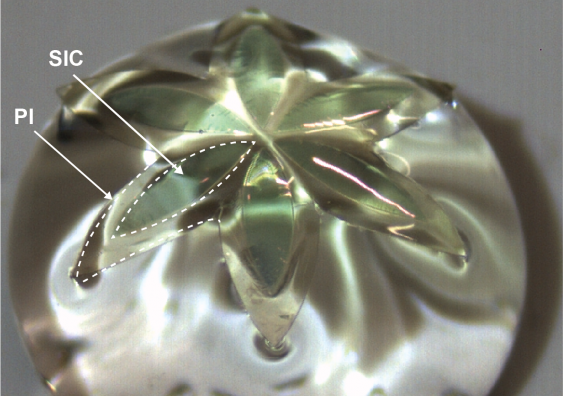
Their new process involves using lithography – a technique that uses light to print tiny patterns – to fabricate wide bandgap semiconductors such as silicon carbide and gallium nitride onto very thin and flexible nanomembranes on a polymer substrate.
Those semiconductor membranes provide sensing, recording, and stimulation functionalities even while being stretched and twisted into any conceivable 3D shape.
They could become an important component of organ-on-chip technology, which is a cutting-edge approach that involves creating miniature versions of human organs on tiny chips.
These chips replicate the functions and structures of organs, allowing scientists to study their behaviour and test the effects of drugs or diseases in a more accurate and efficient manner.
And because organ-on-chip technology allows researchers to mimic the complexity of human organs in lab conditions, it has the potential to eliminate the need to use animals for a wide range of tests and experiments.
“Many people are keen to move towards medical testing on replicated versions of human cells rather than live animals for legal, ethical and moral reasons,” Dr Phan says.
“You can grow 3D cell organs that mimic the organs in a real body, but we also need to develop 3D electrodes to help facilitate that organ-on-chip process.
“Our process allows for an electronic system to be created on a membrane that can be stretched into any 3D shape around the organ-on-chip.”
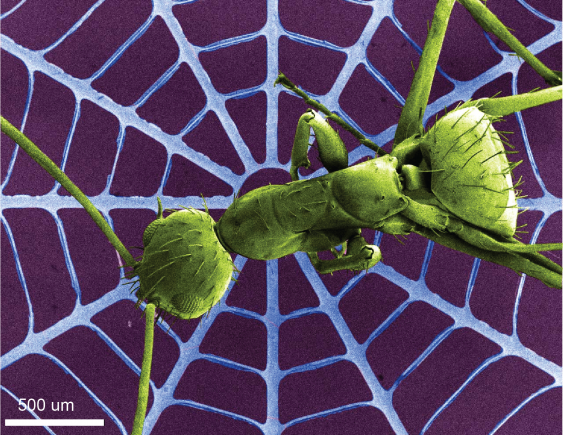
A scanning electron microscope image of a spider web structure made of the new wide bandgap material, featuring a real ant for scale. Image supplied by Thanh-An Truong.
The work is the highlight of interdisciplinary, cross-institutional collaboration between UNSW, Griffith University, UQ, QUT, and their international partners such as Kyung Hee University, University of Southern California, and Northwestern University.
UNSW Scientia Lecturer Dr. Thanh Nho Do, a chief investigator on the project, added: “We use wide bandgap material, which unlike traditional semiconductor materials does not absorb visible light. That means that when scientists want to observe the organ-on-chip through a microscope they can do so, which would not be possible otherwise.
“The electronic system on the membrane also allows a lot of data to be collected while monitoring how the artificial organ is reacting to different things while being tested.”
For this application, the researchers believe it could be a commercial product within three to five years, although they aim to do further work to improve the device even further and integrate additional components such as wireless communication.
In terms of utilising the technology in wearable health monitoring systems, Dr Phan says there is interesting potential for the new process to significantly improve the quality of monitoring, diagnosis, and therapy.
One such function could be a wearable sleeve to help detect and signal alerts regarding the levels of UV radiation a person was being subjected to throughout the day, which could ultimately help lower the instances of skin cancer.
“The wide bandgap material is important in that application because traditional silicon semiconductors have a narrow bandgap and do not absorb UV light,” Dr Phan says.
The UNSW team also propose their new material may be developed further to create implantable biomedical devices where the electrical system can monitor, and influence, neuron signals in real-time.
Although such a device would not likely be available for at least 10 years, the researchers are already planning further tests with the aim of potentially helping people who have epilepsy – a neurological disorder where sudden and uncontrolled bursts of electrical activity in the brain can cause seizures.
“For people with epilepsy, when a seizure is just about to happen the brain will send out unusual signals which are the trigger,” Dr Phan says.
“If we can create an implantable electronic device that can detect those abnormal patterns, it can potentially also be used to apply electrical stimulation to bypass the seizure.”
One of the key challenges that needs to be overcome with regards to implantable devices is how to power such an electronic system.
Researchers at UNSW are therefore also trying to develop a magnetic resonance coupling system that could be integrated with the wide bandgap 3D electronic membranes to wirelessly transfer power through the body via an external antenna.